Don’t Let Bad Data Sabotage Your AI Goldmine
The successful implementation of AI in healthcare presents several key hurdles that enterprises must overcome to unlock their full potential. This is especially true for sectors like healthcare, where data security and integrity are paramount.
Enterprises face a few primary hurdles when embarking on AI initiatives, which can include securing buy-in and willingness to invest from leadership, identifying if and how existing processes can integrate AI, and the availability of skilled professionals to develop and manage AI systems.
While all these points impact the success of AI implementation, the truth is that it is your data readiness for AI (or lack thereof) that can bring progress to a screeching halt.
Related reading: Payers: Is your data ready for AI? Download Here
Challenges to Healthcare AI Data Readiness
In sensitive industries such as healthcare, the stakes of being data-ready are exceptionally high. Data integrity is crucial to essential requirements such as patient safety and diagnostic accuracy – as any data-related error can have serious consequences to patient outcomes.
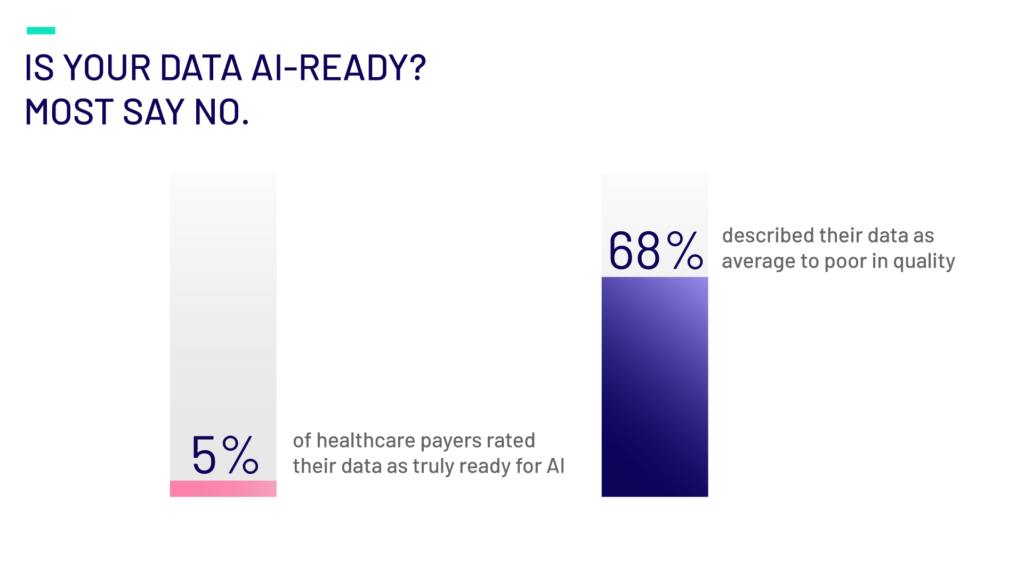
In fact, as per our recent Survey, only 5% of healthcare payers rated their data as truly ready for AI, and 68% described their data as average to poor in quality for AI use.
The healthcare industry faces unique challenges to ensuring good data. Patient data is scattered across various platforms in the healthcare ecosystem who don’t all speak the same language, so to speak. Differing standards and formats across labs, imaging, EHRs, payer systems, etc. can result in fragmented data. This absence of a Single Source of Truth for healthcare data results in data inaccuracies and inconsistencies which leaves providers and payers with unreliable data, impacting the reliability of AI-driven tools and outputs.
Further complicating matters, 75% of payers report persistent data quality issues in core workflows like claims, enrollment, and fraud detection. And a third of organizations still lack data integration across critical workflows. These gaps not only produce sub-par AI outcomes but also increase compliance and cybersecurity risks.
These challenges are complex and shouldn’t be ignored. Addressing them is critical to not only realizing the full potential of AI, but so that your AI initiatives don’t create new or worsen existing problems, ensure regulatory compliance and increase vulnerability against cyber threats.
Complete, uniform, accurate data that can flow between systems and tools, supports the promise of improved patient records, improving administrative efficiencies, and diagnostic support.
Building Trust in Your Data
Trust is a subjective yet vital component to effective AI practices and while it takes years to build trust in brands and people, there’s a prescribed method to improve trust in data:
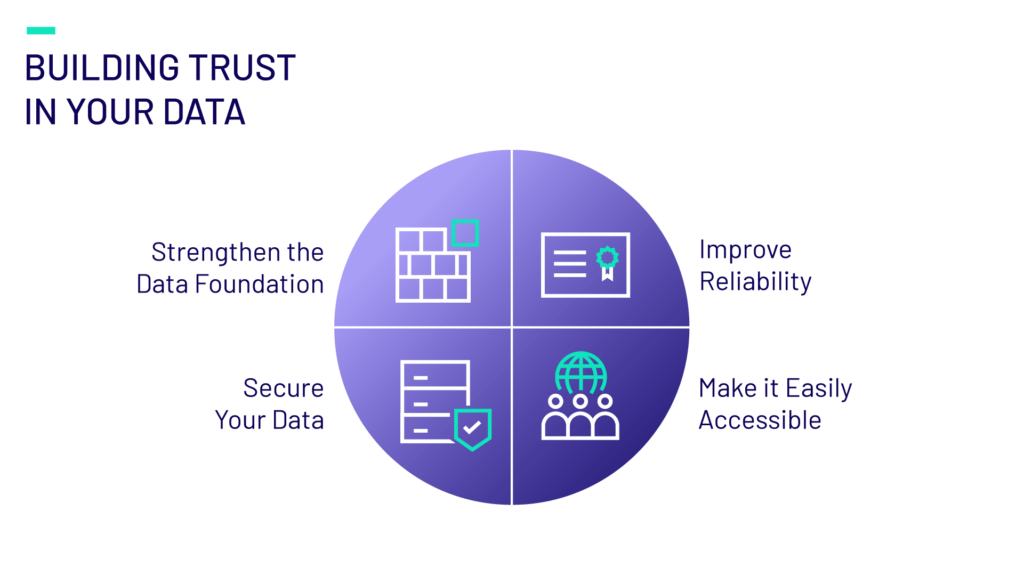
- Strengthen the Data Foundation: Only 5% of payers surveyed have a mature AI roadmap, and 80% are still in the early stages of adoption. Ensure a robust and well-organized data infrastructure as the strategic backbone of your data ecosystem. This includes scalable storage for structured and unstructured data, data models and architecture, and more.
- Improve Reliability: Implement processes to enhance data accuracy and consistency. By implementing interoperability frameworks, investing in data integration platforms, and applying governance models to define ownership and access rights, your data will be ready to produce reliable AI-powered support. Without these, data silos persist—especially when 41% of payers cite data governance as their top challenge, encompassing issues like access control, data quality, and metadata management.
- Secure Your Data: Only 27% of payers surveyed have fully enforced governance policies to ensure compliance. Protect data integrity and confidentiality through robust security measures such as role-based access control, data encryption and regular monitoring and risk assessments.
- Make it Easily Accessible: Ensure that trusted data is readily available to authorized users and systems in order for it to perform at its full potential. Incorporate UX in user interfaces and consider creating dashboards and visualizations to help present complex data in easily digestible mediums.
The Stakes Are High
AI represents a significant opportunity – a potential goldmine – for your business. However, without a foundation of high-quality, trusted data, this goldmine can quickly become a landmine.
Emids Can Help
At Emids, we help healthcare organizations unlock the power of AI by starting at the source: your data. From designing enterprise-wide data strategies to implementing governance frameworks and quality engineering, we help you build the trust your AI depends on.
Digital for All: Why Accessibility Is the Missing Link in Member Engagement
It’s no secret amongst payer executives that digitally engaged members are more likely to schedule preventive care appointments, adhere to prescribed treatments, and are more likely to avoid costly emergency interventions and experience better health outcomes, overall. This enables payers to also reap substantial benefits – particularly in efficiency, cost management, and long-term profitability.
As healthcare payers continue to prioritize digital transformation, ensuring accessibility is essential, not just as a compliance measure, but as a cornerstone of equitable healthcare delivery.
Cognitive, communication and motor decline make it more difficult for older members or those with disabilities to use digital tools designed for the general population. So, when creating digital tools or functions, it’s critical that they be accessible by all members. However, the reality of accessibility across members can vary depending on various demographics such as age and health status. Members of an older demographic may not have the technological skills foundation to navigate digital tools like the general population and the presence of chronic health conditions or disabilities could impact how they use digital tools.
Discovering Unique Member Needs
In a recent Member Engagement survey, we found that overall, 20% of members do not engage with their health insurance plan via digital tools. Amongst the leading reasons for not engaging with their plans’ digital tools include usability issues and technical barriers, which was expressed by 10% and 11% of members, respectively.
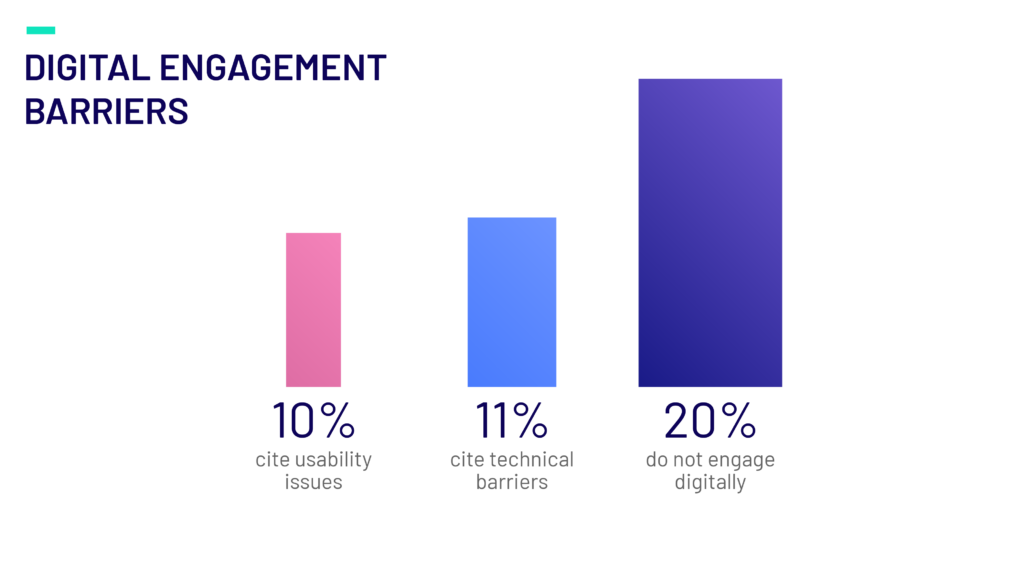
These findings indicate that plans are not doing enough to ensure their tools are accessible to those with lower technical experience or those who may have health conditions that limit their ability to utilize digital tools. By understanding their members, payers can improve accessibility and usability of digital tools to improve overall engagement and ensure all members can experience the benefit of digital engagement functions.
Embedding Accessibility in Digital Transformation
Accessibility must be embedded at the design stage of digital tools and account for the diverse needs of all members from the outset. By adhering to the Web Content Accessibility Guidelines, payers can create digital experiences that are perceivable, operable, and understandable for everyone. This includes providing text alternatives, sufficient color contrast, keyboard navigation, plain language, simplified navigation, and accessible multimedia content. Regular accessibility testing throughout the design, development, and post-launch phases ensures ongoing usability for members with disabilities.
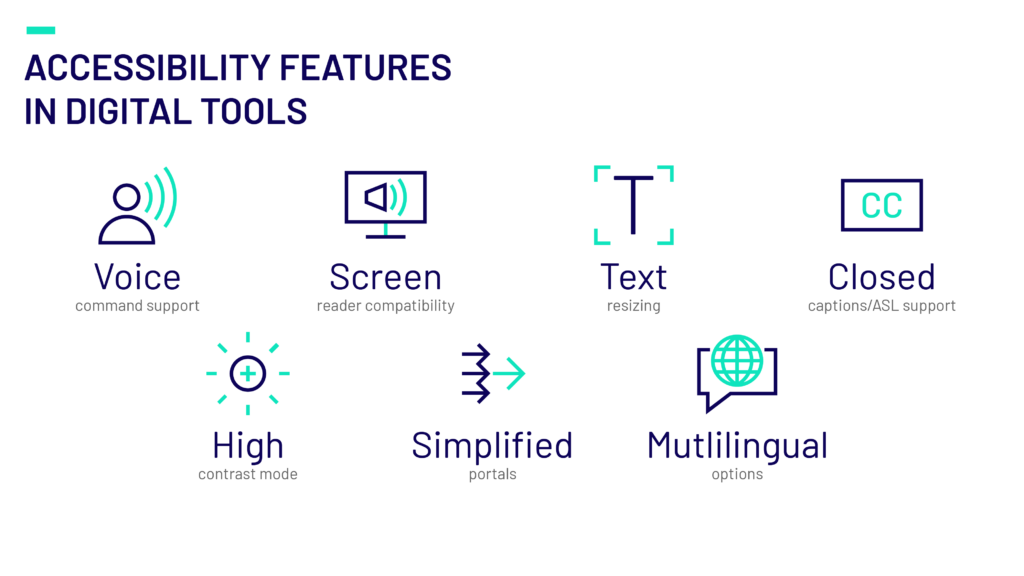
Consider how you can improve usability to meet these unique needs. Offer simplified portals, with easy access to most used functions, such as claims management, provider searches, and plan details. Incorporating accessibility elements such as screen readers in apps, simplified language, ASL-friendly video tools and voice-activated support to meet varied user preferences.
Most importantly, ensure your digital tools have taken accessibility UX considerations in their design and functionality so that members with limited technical experience or health conditions that limit their abilities have equal ability to utilize digital functions and experience their benefit.
Digital Functions for Equitable Healthcare Delivery
Payers can take accessibility to the next level by tailoring digital tools to accommodate members’ specific needs. For instance, members with transportation challenges could benefit from easy-to-use transportation arrangement functions, a tool to arrange for home delivery of prescriptions, or improving access to telehealth.
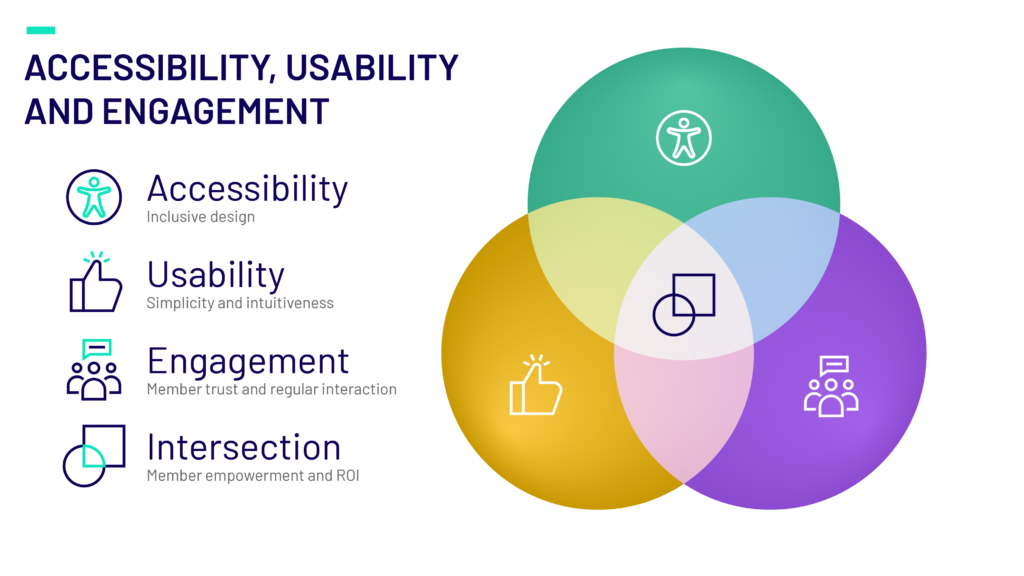
Members are more likely to express loyalty to their plan provider when they perceive them as supportive partners in their health journey. By tailoring members’ toolsets to accommodate their specific needs would not only improve digital engagement, it could improve member retention.
By knowing what your members need, you can build digital tools that empower them to take charge of their health care and realize the value their plan provides.
The ROI of Accessibility in Digital Engagement
Healthcare payers can gain significant benefits by incorporating accessibility into their digital engagement strategies. Accessible platforms improve overall member satisfaction, reduce churn, and expand the reach of engagement tools to a broader audience. Coupled with omni-channel solutions, accessibility ensures payers achieve their goals of delivering equitable, proactive, and personalized care experiences.
Accessibility also drives trust. By demonstrating a genuine commitment to inclusivity, payers solidify their reputations as member-focused organizations invested in the well-being of the communities they serve.
Final Thoughts
Accessibility is not only a legal and ethical responsibility but also a strategic advantage in expanding digital engagement for healthcare payers. By prioritizing user-centric design principles, adopting omni-channel engagement, and implementing ongoing evaluation systems, payers can create a seamless, inclusive experience for all members.
For organizations looking to assess the accessibility of their existing digital tools or seeking expert guidance in redesigning their UX, reach out to learn how we can help you achieve compliance and create meaningful engagement at every touchpoint. Together, we can build a future where accessibility is central to digital health innovation.
From Speed to Scale: Why High-Efficiency Engineering Is Critical for HealthTech Growth
HealthTech leaders today face a growing set of pressures: shorter product cycles, increasing compliance demands, and the constant push to innovate while ensuring system resilience and scalability. In this environment, engineering teams are not just building software—they’re driving business performance.
That’s where high-efficiency engineering becomes critical.
What Is High-Efficiency Engineering?
High-efficiency engineering is an end-to-end methodology designed to maximize impact at every stage of the development lifecycle. By prioritizing streamlined, goal-oriented workflows, it eliminates the bottlenecks that slow down progress and dilute value delivery.
With an emphasis on automation, modular design, data-driven optimization, and built-in quality, this approach enables HealthTech providers to build faster, smarter, and safer—meeting market demand in real-time without compromising compliance or user trust.
The Pillars of High-Efficiency Engineering
Automation and GenAI
Generative AI tools are transforming the way engineering teams operate. They automate repetitive tasks, accelerate debugging, and assist in code generation—cutting down development cycles while enhancing consistency.
“AI enablement will become table stakes across solutions rather than a core differentiator.”
— HealthTech Trends 2025 eBook, Emids
Domain-Aligned Microservices
Replacing complex, monolithic systems with domain-driven microservices brings modularity, flexibility, and speed. These components integrate easily into existing architectures and scale with evolving requirements—whether for patient data exchange, claims workflows, or provider systems.
Data-Driven Decision Making
With advanced analytics embedded into the engineering process, organizations can track engineering performance in real time, identify bottlenecks, and reduce risk. Metrics offer clear visibility into what’s working—and what needs to improve.
Integrated Quality and Compliance
High-efficiency engineering ensures quality is not a separate checkpoint—it’s embedded throughout. Continuous testing, automated validation, and compliance checks reduce manual errors and help teams stay ahead of regulatory requirements like HIPAA, GDPR, and FHIR.
Why It Matters Now
As outlined in the HealthTech Trends 2025 eBook, the sector is shifting toward a performance-first mindset. Organizations that fail to modernize their engineering approach risk:
- Missed go-live deadlines
- Higher rework and support costs
- Lower client satisfaction
- Increased vulnerability to compliance breaches
High-efficiency engineering is not just a way to reduce costs—it’s how leading HealthTech firms are building durable, scalable solutions that meet rising expectations.
Moving Toward Efficiency and Innovation
The HealthTech sector sits at the intersection of urgency and opportunity. Challenges like rising costs, inefficiency, and complex regulation may seem like barriers, but high-efficiency engineering provides a clear path forward. By adopting this approach, your organization can deliver cutting-edge digital solutions while achieving scalability, speed, and measurable ROI.
Take the first step toward transforming your operations. Download our exclusive HealthTech Trends eBook to discover the latest innovations, emerging tools, and practical strategies for long-term success.
The Rise of Autonomous AI in Healthcare: Opportunities and Challenges
Autonomous AI in healthcare is steadily transforming the industry by enhancing patient outcomes, optimizing operations, and strengthening security and privacy. As the technology evolves, HealthTech leaders are continuously refining their applications to unlock new opportunities and enhance existing solutions.
Last week, my colleagues at Emids and I met with HealthTech leaders to explore best practices, insights, and opportunities in autonomous AI. The discussions underscored AI’s growing impact across the healthcare ecosystem.
Key Areas Where Autonomous AI is Driving Value
Patient Engagement & Digital Front Door Strategies
AI-powered virtual assistants, chatbots, and intelligent automation are reshaping patient engagement. These digital front door strategies enhance appointment scheduling, streamline patient outreach, and provide real-time support—improving accessibility and experience.
Clinical Workflow Optimization
AI-driven healthcare tools are addressing serious clinician capacity challenges by optimizing clinical workflows, automating healthcare data integration management, and providing AI-driven diagnostic support. By reducing administrative burdens, autonomous AI allows healthcare professionals to focus on patient care.
Revenue Cycle Management (RCM)
AI-driven revenue cycle management solutions are beginning to impact healthcare financial operations by reducing human errors in medical billing, coding, and collections. Intelligent automation enables faster claim processing and provides actionable insights for revenue forecasting and financial optimization.
Challenges to Overcome
Healthcare Data Integration & Quality
The effectiveness of autonomous AI in healthcare depends on high-quality, well-integrated data. However, as AI expands, integrating structured and unstructured data from multiple sources remains a significant challenge. Ensuring data interoperability and standardization is critical for AI reliability.
Maintaining the Human Touch
While AI-driven healthcare enhances efficiency, successful AI adoption requires balancing automation with meaningful patient-provider interactions. Technology should augment—not replace—the human element in patient care delivery.
Trust & Adoption Among Providers
Healthcare AI adoption depends on trust, which requires transparent and explainable AI models. Clinical validation, regulatory alignment, and clear communication about AI’s role in decision-making are essential to overcoming skepticism—especially regarding AI-generated diagnoses and treatment recommendations.
The Path Forward or Autonomous AI in Healthcare
Autonomous AI has immense potential to reshape healthcare, but successful adoption requires a thoughtful, strategic approach. Trust, transparency, and responsible implementation will be key to ensuring AI’s full impact while maintaining integrity in patient care delivery.
If you’re in the early stages of exploring AI in healthcare, start by identifying where it can drive the most value for your business and clients. Partnering with healthcare AI experts who understand the healthcare landscape can accelerate adoption and ensure meaningful outcomes.
Explore AI Solutions Tailored for Healthcare
At Emids, we specialize in harnessing the power of Generative AI to revolutionize healthcare product development. Our platform, EPulseAI, accelerates product engineering by up to 50%, ensuring faster time-to-market and enhanced accuracy.
Discover how EPulseAI can transform your healthcare solutions.
Bridging Cost Optimization and Innovation with Low-Code and AI
Healthcare payers face the dual challenge of enhancing member services while reducing operational costs in an ever-evolving tech landscape. While many turn to digital solutions, such transformations can be costly and time-consuming. At Emids, we help you leverage low-code platforms to unlock AI’s potential, streamlining operations and improving care delivery—faster and at a fraction of the cost.
The Power of Low-Code and AI in Healthcare
Low-code platforms are a game changer in the digital transformation landscape, offering healthcare payers the means to develop applications quickly and cost-effectively. Low-code solutions utilize pre-built modules and drag-and-drop interfaces, significantly reducing development time and cost while increasing quality. This has enabled healthcare organizations to deploy services at unprecedented speed, allowing them to adapt swiftly to changing market demands and regulatory landscapes.
The integration of AI with low-code platforms allows healthcare payers to harness advanced technologies without the complexity typically associated with AI deployment. AI capabilities can be built into low-code applications, so payers can automate routine processes, derive insights from vast datasets, and deliver personalized member experiences. This synergy between low-code and AI helps payers optimize their operations and improve care delivery, while streamlining AI governance.
Improving Claims Processing
AI-powered claims processing systems built on a low-code platform can save time and minimize errors. One Emids client saw a 40% reduction in processing time and a 25% decrease in errors. This allowed them to reduce their cost margins and enhance member satisfaction through faster claim resolutions. Furthermore, low-code enabled them to deliver the solution in 33% of the original time and cost.
Personalizing Member Engagement
AI can create personalized health engagement plans, tailor recommendations based on member health data. This led to a 30% increase in member participation in wellness programs and a corresponding decrease in chronic condition incidents for an Emids client. Low-code resulted in half the cost and half the time to market than originally forecast.
Automating Fraud Detection
With AI-driven analytics integrated into a low-code framework, fraud detection processes can be automated to identify and mitigate fraudulent activities more effectively. This approach safeguards financial assets and preserves member trust and integrity. By deploying AI within Low-Code based solutions, AI governance is built-in.
Low-code platforms, when combined with AI, offer healthcare payers a powerful toolkit for automation and enhanced care delivery. By streamlining processes, optimizing services, and deploying AI solutions with ease, payers can address operational inefficiencies while meeting the evolving needs of their members. This approach not only drives immediate benefits in terms of cost savings and efficiency but also paves the way for sustainable growth and innovation in the healthcare sector while safely leveraging AI.
To unlock the full potential of low-code and AI in your operations, consider partnering with experts like Emids. With over 20 years of experience transforming healthcare for leading payers, we provide customized solutions tailored to your unique needs. Over just three years, we’ve delivered more than USD 50 million in savings to our customers by deploying intelligent automation. Let us help you bridge the gap between cost optimization and innovation through low-code solutions. Together, we can craft a strategic approach that meets your cost-effective care goals, enhances member care and supports sustainable growth for your plan.
Low-Code, High Impact: Transforming Payer Operations and Member Engagement
For payers, the balance between operational efficiency and rapid innovation has always been a delicate one. Traditional development approaches can be slow, costly, and inflexible, creating a gap between what payers aspire to deliver and what current processes allow. Low-code platforms, however, offer a transformative solution—an approach that promises not only to close this gap but also to empower payers with unprecedented flexibility, speed, and cost savings. By embracing low-code, payers can meet today’s demands and position themselves for tomorrow’s challenges.
Low-Code Solutions Enable Cost Efficiency for Payers
In the healthcare payer industry, maintaining and enhancing legacy systems requires substantial resources, while responding to regulatory changes demands continual innovation.
Here’s where low-code solutions shift the paradigm. Unlike traditional development, low-code accelerates application creation through visual workflows, pre-built components, and model-driven logic, all of which reduce the need for extensive coding. Whether small work-group apps or mission-critical systems of record serving millions of customers, Low-Code can make the impossible, possible. This results in reduced development and maintenance costs, faster deployment cycles, and greater financial flexibility.
Consider the case of claims adjudication, a process central to payer operations. Low-code platforms can automate the claims adjudication workflow, allowing real-time adjustments and reducing manual interventions. By automating claims processing, payers cut administrative costs while delivering faster, more accurate service, enhancing both efficiency and member satisfaction.
Accelerating Time to Market and Innovation
For payers, innovation is not just a competitive advantage; it’s necessary to meet regulatory demands and evolving member expectations. Low-code platforms empower payers to build, test, and launch applications far faster than traditional methods. This acceleration enables payers to pilot new services, deploy member-focused applications, and adapt to market changes with agility.
Data integration is critical for payers, coordinated care. Using low-code, a payer can create interoperable solutions that connect with FHIR and EMR/EHR systems seamlessly. This enables data sharing across the care ecosystem and supports compliance while providing a unified view of member health, helping payers drive faster, more informed decision-making.
Using Low-Code to Deliver AI-Powered Care Insights and Boost Member Engagement
One of the most exciting aspects of low-code is its ability to integrate AI seamlessly into applications. Payers can use low-code platforms to create tools that leverage AI-driven insights, enabling proactive and personalized member engagement.
With low-code, a payer could develop a self-service portal where members receive AI-generated recommendations tailored to their health needs. These insights allow for proactive outreach, such as medication reminders or preventive care suggestions, improving member engagement and supporting better health outcomes.
Scalable, Multi-Device Solutions for Members and Employees
Today’s healthcare members and employees expect flexible, multi-device solutions. Low-code offers payers the ability to design scalable applications that deliver a consistent experience across devices—from desktop to mobile—without requiring extensive development resources. Rather than having a web, iOS, and an Android team, low-code enables a single team to generate device-native experiences with one solution.
For example, A low-code-built member portal provides accessible, on-demand information, enabling members to view plan details, track claims, and manage personal health information seamlessly. Similarly, employee dashboards streamline operational processes by offering insights into service requests, claims status, and member inquiries, all in real-time. This flexibility supports both member satisfaction and operational efficiency.
Streamlining Operational Efficiency through Automation
Low-Code empowers payers to automate repetitive tasks, enhancing operational efficiency and reducing human error. Automated workflows streamline everything from compliance management to HR processes, freeing up resources for strategic initiatives.
By automating document management, low-code helps payers maintain compliance more efficiently, ensuring that audits and quality checks happen without manual intervention. This reduces processing time and ensures that staff focus on high-value tasks, not repetitive manual labor.
The Strategic Value of Low-Code for Payers
Beyond immediate operational benefits, low-code brings lasting strategic value. By reducing dependence on traditional development and freeing up budgets, payers can reinvest in priority areas. Furthermore, with AI and automation capabilities integrated into low-code applications, payers are better equipped to support value-based care models, delivering proactive and personalized member services at scale.
Low-code is not just a faster way to develop applications; it’s a strategic enabler that helps payers close the gap between traditional challenges and future-ready solutions. Embracing low-code allows payers to drive innovation, reduce costs, and enhance member satisfaction. As healthcare’s digital transformation accelerates, low-code provides the foundation for payers to lead with agility, efficiency, and a member-centered approach, ensuring they stay competitive in a rapidly evolving landscape.
Generative AI in Payer Operations: Reshaping Efficiency and Member Satisfaction
As health plans look to implement, optimize, or modernize their core administrative platforms and integrated systems, Generative AI presents a compelling opportunity to drive efficiency and elevate customer satisfaction. But what exactly is Generative AI, and how can payers harness its capabilities to enhance their operations?
Once considered a cautious tech adopter, healthcare today is now at the forefront of a transformative tech boom. Both health systems and health plans are increasingly turning to advanced tools like automation, artificial intelligence, and machine learning to improve efficiencies, cut costs, and enhance the member experience.
Among these innovations, Generative AI is emerging as a powerful solution for payers, offering the ability to reimagine business processes and deliver operational improvements. By automating manual, labor-intensive tasks and processing vast data sets, Generative AI reduces errors, speeds up workflows, and generates insights that improve decision-making. Whether you’re focused on optimizing claims processes, predicting and managing risk in member populations, or enhancing the overall member experience, Generative AI can help streamline operations, deliver faster and more accurate results, and lower costs.
Here are three business areas where Generative AI can enhance efficiencies and deliver real value for your organization:
Enhance Claims Adjudication with GenAI for Faster Processing and Reduced Costs
When a claim is submitted, it either processes through the rules engine based on its configuration or is flagged and pended due to a system edit such as a high dollar amount or other qualifying condition. Claims may also be pended for reasons such as being out-of-network or validation requirements around coordination of benefits. These rules determine whether the claim is automatically processed or routed into a work queue for further review. Generative AI can play a pivotal role by assessing whether there is sufficient medical necessity to continue to hold a pended claim and can even trigger correspondence to validate other payer coverage.
Generative AI enhances the claims review process by pulling claims from work queues and applying an additional layer of analysis before manual intervention is necessary. This not only improves auto-adjudication rates and boosts throughput but also reduces the costs associated with manual intervention and claims that linger, potentially accumulating interest.
By leveraging Generative AI, your organization can streamline the claims process through automatic verification of clinical eligibility and benefits, identification of anomalies like coding errors or fraud, and review of new claims against historical data to determine if additional medical management is needed. This approach enhances efficiency and accuracy in authorization decisions, ultimately decreasing the number of claims requiring manual review and minimizing penalties from delayed processing.
Transform Customer Experience with GenAI for Faster Resolutions and Better Satisfaction
Generative AI can also transform the customer service experience for health plans by providing faster, more accurate responses to member inquiries. As a customer service agent working in a contact center, handling complex benefit questions can often be time-consuming. For example, when a member calls to ask about their remaining physical therapy (PT) visits, the traditional approach requires manually navigating the claims system to check their plan details. With Generative AI, this process becomes far more efficient.
AI can instantly analyze the member’s claims history and benefit plan, quickly providing information such as how many PT visits have been used and how many remain. This allows agents to deliver insights to the member faster, enhancing the overall experience. Instead of spending time manually searching through records, agents are automatically fed relevant data, enabling them to be proactive rather than reactive.
This improvement in efficiency leads to faster resolutions, better call throughput, and the potential to reduce call volume altogether. Members receive the information they need more quickly, leading to higher customer satisfaction (CSAT) scores and an overall positive experience with the health plan. In turn, this helps payers strengthen their member relationships and improve operational efficiency.
Revolutionize Care Management and Population Health with GenAI
You can also greatly optimize your approach to care management and population health by leveraging Generative AI to implement proactive, data-driven strategies targeting chronic diseases like diabetes, COPD, asthma, and more. The primary goal in care management is to support sicker populations and effectively manage complex, chronic conditions. By integrating Generative AI with care management platforms and population health tools, health plans can monitor and address these conditions more efficiently.
For example, in diabetes management, health plans often begin by establishing clear benchmarks for a target cohort, such as identifying members with both diabetes and obesity. Once these benchmarks are set, Generative AI can conduct disease surveillance by analyzing claims histories and population health data. This enables AI to identify patterns not only in members already diagnosed with diabetes but also in those at risk, allowing care managers to intervene proactively before issues escalate into more serious and costly conditions.
Additionally, by examining claims histories and identifying trends in members’ health, Generative AI can uncover factors that contribute to complex diagnoses like diabetes combined with obesity. Armed with this information, health plans can implement preventative measures, such as outreach and coaching for pre-diabetic members. This proactive strategy can enhance health outcomes and reduce overall care costs by preventing the progression of chronic conditions. Moreover, health plans can track the impact of Generative AI in preventing these diagnoses among at-risk populations, ultimately improving population health outcomes.
Getting Started: Using Generative AI to Create Actual Insights

These are just a few examples of the numerous business cases where Generative AI can significantly enhance your operations, elevate member satisfaction, and drive cost savings. The potential applications of Generative AI are vast, spanning from member outreach and onboarding to pricing and benefits design. As a health plan, your immediate challenge is determining where to begin your journey with Generative AI.
To tackle this challenge effectively, it’s essential to focus on use cases that can deliver immediate, measurable benefits. Every health plan operates with its own unique, customized systems, so the first step is to identify areas where Generative AI can address high-cost, high-volume challenges. For instance, if your organization processes tens of thousands of claims annually in specific categories like coordination of benefits for member coverage, these manual interventions may be costing significant time and money. Such repetitive, labor-intensive processes are prime candidates for AI-driven optimization.
Once you’ve identified the problem area, the next step is to partner with an expert team like Emids. We can help you explore how Generative AI can drive operational efficiency and improve your bottom line. From discovery to implementation and ongoing support, we’ll guide you through each phase to ensure the technology is seamlessly integrated and delivers lasting results.
Contact Emids today to learn how Generative AI can streamline your payer operations and boost member satisfaction.
Transforming Healthcare Payer Operations with Intelligent Automation
Healthcare payers face mounting challenges as they strive to meet regulatory requirements, manage costs, and maintain quality service. Regulatory changes and the recalibration of Star ratings by CMS directly impact revenue streams and reputational standings. Meanwhile, healthcare costs continue to rise due to medical inflation and increased service demand, putting further strain on operational budgets.
According to Gartner’s 2024 Hype Cycle for U.S. Healthcare Payers, 67% of payers rank margin improvement as a top three priority, and investments in AI and automation are expected to reduce industry costs by 15-20%. Operational inefficiencies—such as manual processing of claims, slow member service responses, and outdated systems—drive up Per Member Per Month (PMPM) costs and hinder margin improvement.
To address these pressures, payers must move beyond short-term cost-cutting measures and adopt sustainable solutions. Automation offers a strategic approach to streamline operations, eliminate inefficiencies, and free up resources for innovation and member engagement. By automating manual processes, payers can enhance their operational efficiency and future-proof their businesses.
Unlock Efficiency with Intelligent Automation in Healthcare
Intelligent automation goes beyond simple task automation; it involves the integration of advanced technologies like artificial intelligence (AI) and machine learning (ML) into business processes. This approach enables healthcare payers to automate complex tasks, improve accuracy, and enhance decision-making.

By eliminating manual interventions, payers can achieve faster response times, reduced errors, and improve compliance with regulatory standards. For example, intelligent automation can significantly increase claims auto-adjudication rates, reduce medical management costs, and enhance member and provider experiences. Here are some of the top ways that intelligent automation can optimize operations.
Streamline Claims Processing with Automation
Traditional claims processing is often labor-intensive and prone to errors, leading to delays and increased costs. Automation can streamline claims adjudication by automatically verifying eligibility, processing claims, and detecting potential fraud. This reduces the time and resources required for manual review, while increasing accuracy.
Automate Member Enrollment and Enhance Member Service
Automating member enrollment processes can simplify onboarding and enhance member experiences. Intelligent automation can also improve self-service capabilities, allowing members to access information and services quickly and easily. This leads to increased member satisfaction and reduced administrative costs.
Provider and Network Management Automation
Managing provider networks involves complex tasks such as credentialing, contract management, and network adequacy assessments. Automation can streamline these processes by automating data collection, verification, and analysis, ensuring compliance and improving provider relationships.
Making Automation Intelligent for Healthcare Payers
Implementing automation requires careful planning and strategic execution. Here are the essential steps healthcare payers need to take to successfully automate their operations:
- Assess Current Processes: Begin by conducting a comprehensive assessment of existing manual processes. Identify areas that are labor-intensive, error-prone, and time-consuming. This analysis will help prioritize automation initiatives and determine where automation can deliver the most significant impact.
- Define Automation Goals: Clearly define the goals and objectives of automation. Determine what specific outcomes you want to achieve, such as reducing costs, improving accuracy, or enhancing member experiences. Align these goals with your organization’s strategic priorities to ensure successful implementation.
- Select the Right Automation Tools: Choose automation tools and technologies that fit your organization’s needs and capabilities. Consider factors such as scalability, integration capabilities, and ease of use. Collaborate with technology partners and vendors to identify solutions that align with your automation strategy.
Building Resiliency with Automation to Future-Proof Your Business
Automation is not just about addressing current challenges, it’s about building resilience and preparing for the future. In an industry characterized by rapid changes and increasing complexity, healthcare payers need flexible and scalable solutions. Automation provides the agility required to adapt to changing regulations, emerging technologies, and evolving member expectations.
By automating manual processes, payers can create a sustainable foundation for growth, innovation, and continuous improvement. Automation enables organizations to scale their operations efficiently, expand service offerings, and deliver high-quality care to members. It empowers payers to stay ahead of the competition and meet the demands of a dynamic healthcare environment.
Partnering with Technology Providers for Successful Automation
Partnering with experienced technology providers can significantly enhance the success of automation initiatives. Technology partners bring specialized expertise, industry insights, and proven methodologies to the table. They can guide healthcare payers through the entire automation life cycle, from strategy development to implementation and optimization.
Collaborating with trusted partners allows payers to leverage cutting-edge technologies, access industry best practices, and accelerate their automation journeys. By tapping into the knowledge and resources of technology partners, payers can achieve faster results and realize the full potential of automation.

In a project with a leading Blues Health Plan, our automation project led to 500,000+ hours over the last 3 years with 375+ automations, delivering a 3X ROI.
Keep in mind that automation is just one powerful tool in the arsenal for optimizing payer operations. If you are interested in learning more about automation or discovering other opportunities for payers to achieve significant cost optimization within your operations, download our comprehensive free eBook. This resource offers insights and strategies tailored to help you navigate the complexities of cost management. Connect with us for personalized advice and support tailored to your specific needs.
Optimizing Claims Workflows: Are Inefficiencies Costing Your Health Plan Money?
How Well Do You Know Your Data? Is It Costing You Money?
Health plans operate in a complex environment where every claim tells a story. But how well do you truly understand that story? The reality is that inefficiencies in claims processing could be costing you more than you realize.
Start by evaluating key metrics: What is your auto-adjudication rate? What does your PEND ratio look like? How many claims required multiple reviews before payment or were resubmitted for adjustments? If any of these figures seem higher than expected, it might indicate deeper inefficiencies within your claim workflows.
At Emids, we help health plans optimize their core administrative systems (CAS) and streamline data integration, improving both accuracy and speed. By addressing inefficiencies, cleaning up claim workflows, and automating manual processes, you can reduce operational costs and turn potential losses into savings.
The Critical Role of Optimizing Claims Systems
Health plans rely on the expectation that claims, especially routine ones, should flow smoothly through their systems. Stopgaps and protections are in place to flag high-dollar claims or risky procedures, ensuring they receive the necessary scrutiny. However, if routine office visits or straightforward claims are halted, it’s often a sign of deeper issues. Operational disruptions such as incorrect pricing setups, missing modifiers, or misaligned coding may be forcing unnecessary manual interventions.
Read more: Fixing Broken Core Administrative Systems for Future Growth
The key to overcoming these challenges lies in creating a robust coding framework that minimizes such disruptions. Optimizing your claims data flow not only boosts efficiency but also ensures your reporting is accurate and actionable.
The Importance of Visibility in Claims Processing
For a health plan to operate effectively, it needs complete visibility into its claims data, especially for pended claims. Knowing why claims are being held up—for example, due to an incorrect pricing setup or another configuration error—empowers your team to address bottlenecks quickly. The faster you identify and resolve issues, the more operational efficiency you gain.
Automation plays a crucial role here. By automating tasks like report generation and claims processing, health plans can free up resources for more value-driven activities. When manual intervention is required for tasks that could be automated, it drains resources and inflates operational costs.
The High Cost of Manual Claims Processing
Claims processors are often evaluated based on their ability to handle large volumes of claims in a limited timeframe. Their focus should ideally be on reviewing claims for medical necessity. Yet, too often, they get bogged down by routine tasks stemming from configuration errors. This misallocation of time and resources impacts both productivity and costs.
Moreover, many states require that claims be paid within a specific timeframe, sometimes accompanied by mandatory interest rates. A backlog of manual claims can lead to interest penalties, driving up costs even further.
Another common stumbling block is coordination of benefits (COB). For example, if a member holds coverage with another plan but is incorrectly designated as primary on your plan, this can unnecessarily delay the claims process. Rather than holding up claims for lengthy investigations, optimizing workflows ensures quicker resolutions and fewer operational hiccups.
Turn Claims Processing Inefficiencies into Cost Savings
By streamlining claim workflows and optimizing your CAS for efficient reporting and processing, health plans can significantly enhance both speed and accuracy. This transformation shifts potential operational losses into measurable savings.
At Emids, we specialize in empowering health plans to unlock the full potential of their data. Through automation, improved visibility, and enhanced data flows, we help you turn inefficiencies into competitive advantages.
Our comprehensive configuration audit includes an in-depth review of provider contracts, member benefit requirements, configuration settings, and test results. Our team analyzes decisions made during the configuration process to identify root causes of existing issues and deliver actionable recommendations for improvement. We then develop and implement a customized plan to optimize your claim workflow, ensuring greater efficiency and effectiveness.
To learn more about how you can partner with our team to improve your claim workflow and save time and money, contact us today.
Navigating Cloud Adoption: A Strategic Approach to Cloud Cost Management in Healthcare
Healthcare organizations are under significant pressure to manage costs while adopting transformative technologies like cloud computing. The cloud promises scalability, flexibility, and a consumption-driven model, which is especially attractive as healthcare data volumes grow.
However, despite these benefits, the rapid adoption of cloud technologies has exposed gaps in cost management, eroding return on investment (ROI) and leaving healthcare organizations grappling with unforeseen expenses.
This article, based on insights from the first episode of Emids’ Expert Talks series, explores the key drivers behind cloud adoption in healthcare and presents strategies for managing costs and maximizing value. As healthcare organizations embark on their cloud journeys, they must approach this transition with a strategic mindset, focusing on financial governance, data integration, and long-term planning.
Cloud Adoption as an Industry Imperative
Cloud adoption has moved beyond being just a technology upgrade; it is now a strategic necessity for healthcare organizations. The industry’s reliance on vast amounts of data—whether from claims, labs, or patient records—makes it essential to leverage cloud infrastructure to handle and process this information efficiently. The ability to scale and adjust quickly to demand fluctuations offers healthcare providers the flexibility they need to address operational and clinical challenges.
Healthcare organizations are also shifting toward a more patient-centric model, unifying data across multiple touchpoints to create comprehensive member views. This unified approach is critical for delivering personalized care and driving insights through analytics and business intelligence. However, to fully realize these benefits, organizations must carefully plan their cloud adoption strategy, addressing data dependencies and ensuring that their cloud migration is seamless and well-architected.
The Rising Cost Challenge
Healthcare organizations accustomed to traditional CapEx-based models often struggle to adjust to the consumption-driven nature of cloud services. With cloud, organizations pay for what they use, but without proper oversight and financial governance, costs can escalate, threatening the ROI.
To address this, healthcare organizations must treat cloud migration as a long-term transformative journey, not a one-time event. The complexity of legacy systems, disparate data sources, and ongoing digital transformation efforts all contribute to the challenges organizations face in managing costs during cloud adoption and beyond.
It’s important to keep cost at the forefront while architecting applications and developing consumption patterns and create a right balance between storage and compute cost.
Implementing a FinOps Approach for Financial Governance
Financial governance is key to controlling cloud costs, and many healthcare organizations are turning to FinOps (Financial Operations) programs to guide their cloud strategy. A FinOps approach focuses on bringing together IT, finance, and business leaders to create a structured framework for budgeting, forecasting, and cost optimization.

Key aspects of a successful FinOps program include:
Budgeting and Forecasting
Accurate forecasting is essential for controlling cloud costs. This involves predicting the workloads and data volumes that will be processed, as well as accounting for compliance requirements, testing programs, and business events. By forecasting cloud usage effectively, organizations can set realistic budgets and avoid surprises.
Monitoring and Cost Management
Continuous monitoring of cloud usage is crucial to identifying cost overruns and ensuring that cloud resources are used efficiently. Healthcare organizations should implement mechanisms for tracking consumption patterns and assigning ownership for cloud services to individual teams. This enables proactive cost management and allows organizations to adjust their strategies in real-time.
Optimizing Cloud Resources
Cost containment involves optimizing the cloud architecture to avoid overprovisioning and ensure that resources are being used efficiently. Organizations must also be aware of contractual opportunities, such as slot reservations or discounts from cloud providers, that can help reduce costs.
Change Management
Effective change management is necessary to course-correct when costs deviate from the plan. Organizations should have processes in place to tweak cloud strategies, optimize workflows, and address inefficiencies before they escalate.
The Importance of Cross-Functional Collaboration
A successful cloud migration requires collaboration across the entire organization, not just within IT. Executive sponsorship from the C-suite is critical to ensuring that cloud initiatives are aligned with the broader business strategy. Finance and IT teams must work closely to establish KPIs for cloud efficiency and performance, while business leaders must understand how cloud investments align with long-term goals.
Healthcare organizations must also recognize that cloud adoption requires business process transformation. Moving to the cloud may necessitate rethinking traditional workflows, integrating new technologies like APIs, and adopting industry standards such as FHIR and OMOP to ensure data interoperability and consistency.
Measuring Success and Ensuring Long-Term Value
As healthcare organizations progress through their cloud journeys, it’s important to measure success not only in terms of cost savings but also through improvements in operational efficiency and patient outcomes. Key performance indicators (KPIs) such as cost per terabyte of data storage or processing provide valuable insights into the efficiency of cloud operations. Monitoring these metrics allows organizations to make data-driven decisions and adjust their strategies as needed.
The ultimate goal of cloud migration is to enhance the total cost of ownership (TCO) while speeding up time to business value. By carefully managing dependencies, leveraging the right cloud services, and maintaining a focus on long-term objectives, healthcare organizations can ensure that their cloud investments deliver the desired outcomes.
Today, cloud adoption offers healthcare organizations significant opportunities for innovation, scalability, and improved operational efficiency. However, without a strategic approach to cost management and financial governance, the benefits of cloud can be undermined by escalating expenses. By implementing a robust FinOps program, fostering cross-functional collaboration, and focusing on long-term value, healthcare organizations can navigate the complexities of cloud migration and unlock the full potential of their cloud investments.
The journey to the cloud is a transformative process that requires careful planning, execution, and ongoing management. For healthcare organizations, success lies in treating cloud migration not just as a technology upgrade but as a strategic enabler of business value, one that positions them for future growth and innovation in an increasingly digital world.

